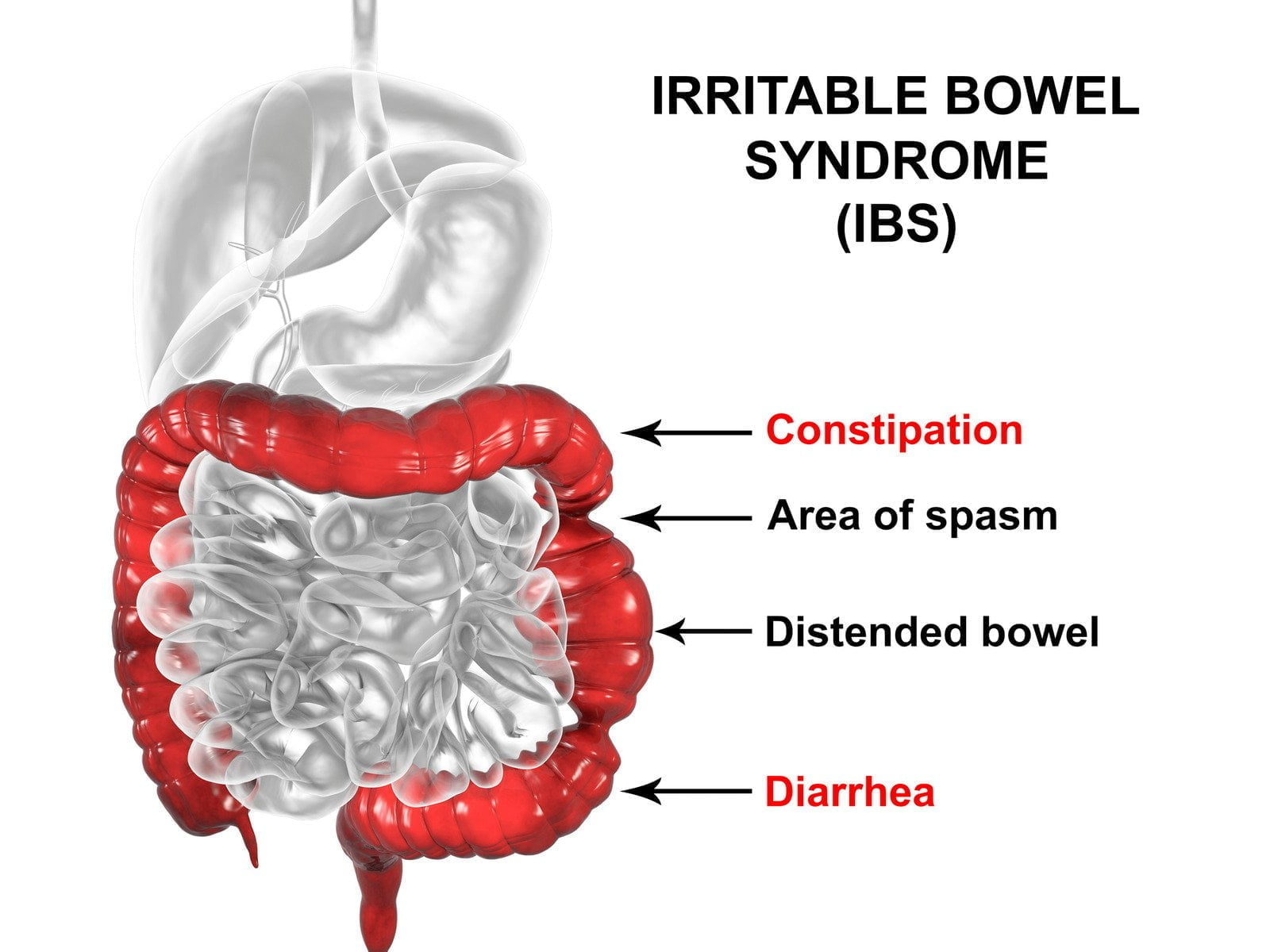
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder that affects the large intestine (colon). It is characterized by various symptoms that can vary in intensity, causing discomfort and disruption to daily life. IBS is a chronic condition and is diagnosed based on the presence of certain symptoms, often after other digestive disorders have been ruled out.
Symptoms of IBS
Irritable Bowel Syndrome (IBS) is characterized by a wide range of symptoms that can vary in intensity from person to person. These symptoms can often mimic those of other digestive disorders, making understanding the specific signs associated with IBS important. Here are the various symptoms of IBS and their potential impact on individuals’ daily lives:
– Abdominal Pain and Discomfort:
One of the symptoms of IBS is abdominal pain or discomfort. This pain can occur anywhere in the abdomen and is often described as cramping, sharp, or dull. The severity of the pain can vary, and it may be relieved temporarily after a bowel movement.
– Bloating and Gas:
Bloating is a feeling of fullness or tightness in the abdomen caused by excess gas. Gas can lead to discomfort, swelling, and audible noises within the stomach or intestines. Bloating can fluctuate throughout the day and may worsen after eating certain foods.
– Altered Bowel Habits:
IBS can lead to changes in bowel habits, including diarrhea, constipation, or alternating between the two. Diarrhea-predominant IBS (IBS-D) is characterized by loose stools and an increased frequency of bowel movements. Constipation-predominant IBS (IBS-C) involves infrequent and difficult-to-pass stools.
– Mucus in Stool:
Some individuals with IBS may notice mucus in their stool. While the digestive tract naturally produces mucus, excessive amounts could indicate irritation or inflammation.
– Urgency and Incomplete Evacuation:
People with IBS may experience a sense of urgency to have a bowel movement, often leading them to rush to the restroom. Additionally, a feeling of incomplete evacuation, where it seems that not all stool has been passed, is common.
– Alternating Bowel Habits:
Mixed IBS (IBS-M) involves a combination of both constipation and diarrhea. This can lead to unpredictable and alternating bowel habits, causing significant discomfort and distress.
– Fatigue and Disrupted Sleep:
Chronic symptoms of IBS, particularly those associated with diarrhea or frequent bowel movements, can lead to fatigue and disrupted sleep. Frequent nighttime awakenings to use the restroom can negatively impact sleep quality.
– Emotional Impact:
The symptoms of IBS can have a profound emotional impact, causing stress, anxiety, and even depression. The unpredictable nature of symptoms and potential social discomfort can contribute to psychological distress.
– Triggers and Flare-Ups:
Individuals with IBS often identify specific triggers that worsen their symptoms. These triggers can include certain foods, stress, hormonal changes, etc. Symptom flare-ups can be unpredictable and vary in duration.
– Pain Relieved by Bowel Movements:
Some individuals with IBS find relief from abdominal pain or discomfort after a bowel movement. This phenomenon is unique to IBS and can provide temporary respite from discomfort.
Causes and Triggers of Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a multifactorial condition, which means that a combination of factors influences its development and exacerbation. These factors can vary from person to person, making IBS a complex disorder to understand. Here are the causes and triggers that play a role in the onset and aggravation of IBS symptoms.
– Gut-Brain Interaction:
One key factor in IBS is the connection between the gut and the brain. This is known as the gut-brain axis, and it involves bidirectional communication between the central nervous system and the digestive tract. Stress, anxiety, and emotional factors can impact gut motility and sensitivity, triggering or worsening IBS symptoms.
– Altered Gut Motility:
Individuals with IBS often experience abnormal gut motility patterns, leading to accelerated or slowed food movement through the digestive tract. This can result in diarrhea-predominant (IBS-D), constipation-predominant (IBS-C), or mixed (IBS-M) symptoms.
– Gut Sensitivity and Pain Perception:
People with IBS tend to have heightened sensitivity to pain and discomfort within the gastrointestinal tract. Even mild stimuli that wouldn’t usually cause discomfort can trigger pain and discomfort in those with IBS.
– Intestinal Inflammation:
While IBS isn’t characterized by the same inflammation seen in conditions like inflammatory bowel disease (IBD), some individuals with IBS may have low-level inflammation in the intestines. This inflammation can contribute to heightened sensitivity and symptoms.
– Gut Microbiota Imbalance:
The gut microbiota, a diverse community of microorganisms in the digestive tract, plays a crucial role in digestive health. An imbalance in the composition of these microbes, known as dysbiosis, has been associated with IBS symptoms. The specific role of the microbiota in IBS development is an area of ongoing research.
– Food Sensitivities and Triggers:
Certain foods or food components can trigger or exacerbate IBS symptoms. These triggers can vary widely from person to person but often include high-fat foods, caffeine, alcohol, dairy products, artificial sweeteners, and certain types of carbohydrates (FODMAPs).
– Hormonal Factors:
Hormonal changes, particularly in women, can influence IBS symptoms. Many women report worsening symptoms during their menstrual cycle, indicating a hormonal connection.
– Stress and Anxiety:
Stress and anxiety are known triggers for IBS symptoms. Psychological distress can lead to changes in gut motility, increased gut sensitivity, and altered pain perception.
– Infections and Gastroenteritis:
Some individuals develop IBS after experiencing a gastrointestinal infection known as post-infectious IBS (PI-IBS). The infection can lead to long-term changes in gut function and sensitivity.
– Genetic and Environmental Factors:
Evidence suggests that genetics and environmental factors may play a role in predisposing individuals to develop IBS. Family history of IBS and exposure to early life stressors can contribute to its development.
Types of Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a complex gastrointestinal disorder characterized by various symptoms affecting the digestive system. These symptoms can manifest differently in different individuals, leading to the classification of IBS into various types. Understanding these types can help individuals and healthcare professionals effectively manage and treat the condition. Here, we delve into the three main types of IBS:
– IBS-D (Diarrhea-Predominant):
In IBS-D, individuals experience frequent episodes of diarrhea that may accompany urgency, watery stools, and a feeling of incomplete bowel movements. Abdominal pain and discomfort are common, often relieved by a bowel movement. The exact cause of IBS-D is complex, involving factors like increased gut sensitivity, altered gut motility, and possible microbiota imbalances.
– IBS-C (Constipation-Predominant):
People with IBS-C have infrequent and difficult-to-pass bowel movements. Their stool may be hard, dry, and lumpy, and they often report straining during defecation. Abdominal pain and discomfort are prevalent, and relief may not always be achieved after a bowel movement. IBS-C can result from altered gut motility, excessive water absorption in the intestines, and other contributing factors.
– IBS-M (Mixed-Type):
IBS-M combines symptoms of both diarrhea and constipation. Individuals with IBS-M experience alternating periods of diarrhea and constipation, often without a predictable pattern. Abdominal pain and discomfort can occur during both phases. The alternating nature of this type can make it particularly challenging to manage, as treatment approaches must address both extremes.
Diagnosis of Irritable Bowel Syndrome (IBS)
Diagnosing Irritable Bowel Syndrome (IBS) can be complex due to its varied symptoms and the need to rule out other potential gastrointestinal disorders. Healthcare professionals systematically evaluate and diagnose IBS, ensuring patients receive appropriate care and treatment. Here’s a closer look at the diagnostic process:
– Medical History and Symptom Evaluation:
The journey to an IBS diagnosis often begins with a detailed medical history. Healthcare providers will inquire about the patient’s symptoms, including the nature of abdominal pain or discomfort, changes in bowel habits (diarrhea, constipation, or alternating), the presence of mucus in stools, and any factors that trigger or alleviate symptoms. A symptom-based approach is vital, as IBS is primarily diagnosed based on the presence of specific symptoms over time.
– Rome Criteria:
One key tool used in diagnosing IBS is the Rome criteria. These are established guidelines that outline specific symptom patterns that must be present for a diagnosis of IBS. The criteria emphasize the duration and frequency of symptoms, ensuring that they are chronic and recurrent. Additionally, the symptoms should not be indicative of other gastrointestinal conditions.
– Physical Examination:
During a physical examination, healthcare professionals assess the abdomen for tenderness, bloating, and discomfort. Because the absence of physical abnormalities is common in IBS, the diagnosis primarily relies on the patient’s reported symptoms.
– Laboratory Tests:
Laboratory tests may be conducted to rule out other potential causes of gastrointestinal symptoms. Blood tests can help identify inflammation, anemia, thyroid disorders, and other conditions. Stool tests may be performed to check for infections, parasites, and other abnormalities.
– Imaging Studies:
Imaging studies such as abdominal X-rays, CT scans, or MRIs may be ordered to ensure there are no structural abnormalities or other conditions that could be causing the symptoms. These tests help confirm that the symptoms align with IBS and not another underlying condition.
In some cases, healthcare providers may recommend additional tests if there are atypical symptoms or if they suspect another condition. These may include colonoscopy or endoscopy to visualize the gastrointestinal tract and rule out more serious conditions like inflammatory bowel disease (IBD).
Management and Treatment of IBS:
While IBS has no cure, management strategies aim to alleviate symptoms and improve quality of life. Here’s an overview of the management and treatment options for IBS:
1. Lifestyle Modifications:
- Dietary Changes: Modifying one’s diet is often a key aspect of managing IBS. This can include identifying trigger foods that exacerbate symptoms and avoiding or limiting their consumption. Common triggers may include certain carbohydrates (FODMAPs), spicy foods, fatty foods, caffeine, and artificial sweeteners.
- Fiber Intake: Increasing dietary fiber can help regulate bowel movements and alleviate symptoms of constipation and diarrhea. Soluble fiber, particularly in oats, beans, and fruits, is particularly beneficial.
- Meal Planning: Eating smaller, more frequent meals can prevent digestive system overload and reduce symptoms like bloating and discomfort.
- Hydration: Staying adequately hydrated is important for maintaining healthy digestion and preventing constipation.
2. Medications:
- Antispasmodic Medications: These medications help relax the digestive tract muscles, reducing cramping and discomfort.
- Antidiarrheal Medications: These medications can help control bowel movements and reduce urgency in individuals with IBS-D (diarrhea-predominant).
- Laxatives: In cases of IBS-C (constipation-predominant), laxatives may be recommended to alleviate constipation.
- Probiotics: Certain strains of probiotics have shown promise in improving gut health and managing IBS symptoms by promoting a balanced gut microbiome.
3. Stress Management:
- Stress and anxiety can exacerbate IBS symptoms. Deep breathing, meditation, yoga, and mindfulness can help manage stress and improve digestive well-being.
Goodness Digestive Enzymes are designed to assist the body in breaking down food into absorbable nutrients. A blend of enzymes, including amylase, protease, lipase, and others, helps break down carbohydrates, proteins, and fats.
For individuals with IBS, Goodness Digestive Enzymes can alleviate symptoms by:
- Enhancing digestion and absorption of nutrients
- Reducing abdominal bloating and discomfort
- Supporting a balanced gut microbiome
- Minimizing triggers that cause IBS flare-ups
Integrating Goodness Digestive Enzymes into the daily routine could support managing IBS with dietary adjustments, medications, and other therapeutic strategies.
Conclusion:
Irritable Bowel Syndrome is a complex and chronic gastrointestinal disorder that can significantly impact an individual’s quality of life. While there is no one-size-fits-all solution, combining dietary, lifestyle and medical interventions can help manage symptoms and improve well-being. If you suspect you have IBS, it’s essential to consult a healthcare provider for a proper diagnosis and personalized treatment plan.
-
Product on sale
 Goodness Digestive EnzymesOriginal price was: $ 29.95.$ 25.95Current price is: $ 25.95.
Goodness Digestive EnzymesOriginal price was: $ 29.95.$ 25.95Current price is: $ 25.95.